Introduction:The underlying pathophysiology of severe COVID-19 involves cytokine storm syndrome that is associated with an elevation of immunoinflammatory cytokines [1]. This hyper-inflammatory state has been implicated with coagulopathy among severely sick patients with COVID-19. Inflammation and coagulopathy are interlinked processes [2]. Coagulopathy has been associated with high mortality in COVID-19 patients [3]. LMWH is traditionally used for its anticoagulant and antithrombotic properties, however, its anti-inflammatory effect has not been fully elucidated. A study done by Shastri et al. suggested that LMWH can inhibit the release of different cytokines (IL-4, IL-5, IL-13, and TNF-α) [4]. Recent retrospective studies on COVID-19 illustrated that the LMWH (40-60 mg, subcutaneously every day) was associated with better prognosis as measured by (28 days of survival) in severely sick patients meeting sepsis-induced coagulopathy (SIC≥4) criteria compared to nonusers [5]. The potential role of escalated/therapeutic LMWH (1mg/kg/subcutaneously every 12 hours) remains unclear. This study involves a retrospective analysis of the potential role of an escalated dose of LMWH to alter the hyper-inflammatory state in hospitalized patients with COVID-19 and compared outcomes to those patients who received a low dose (40-60 mg, subcutaneously every day) of LMWH.
Methods:Adult patients with confirmed SARS-CoV-2 infection by nasopharyngeal (NP) polymerase chain reaction (PCR) who were hospitalized from March 1st to April 20, 2020, were included. They were divided into two cohorts based on the dose of LMWH; cohort 1 (40-60 mg, subcutaneously every day) and cohort 2 (1mg/kg/subcutaneously every 12 hours). Categorical variables were compared by conducting a chi-square test or Fisher's exact test while continuous ones were compared by conducting a median two-sample test.
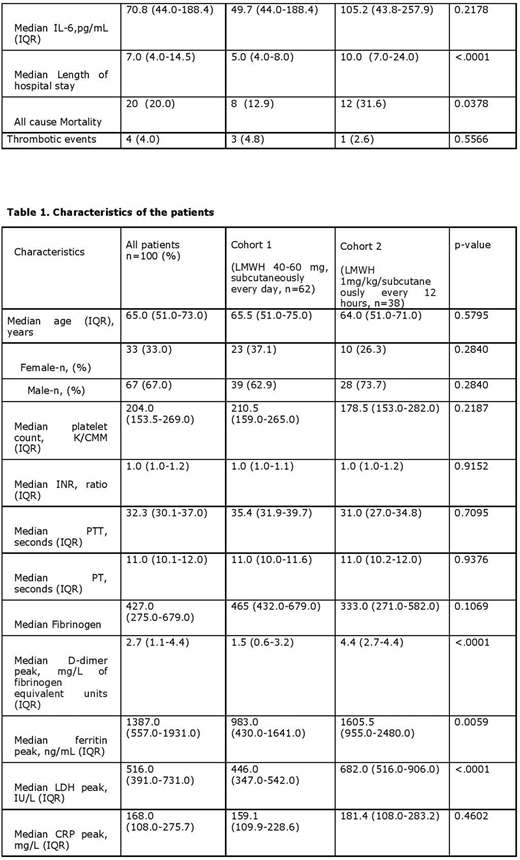
Results:The median values of PT, PTT, INR, CRPmax, LDHmax, ferritinmax, D-dimermax, are mentioned in table 1. Incidence of thrombotic events (deep venous thrombosis, ischemic stroke, pulmonary embolism) was higher in cohort 1 (n=3, 4.8%) compared to cohort 2 (n=1, 2.6%). Cohort 2 had a higher number of patients who received ICU level of care (n=24) compared to the 6 patients in cohort 1. Out of 24 patients in cohort 2, 18 patients received invasive mechanical ventilation. The median value of length of stay in the hospital (10.0 days) and all-cause mortality (31.6 %) were higher in cohort 2 as compared to cohort 1 (p<0.05).
Discussion:Infections have the ability to trigger systemic inflammation [6]. The interplay between the host system and its response to foreign pathogens can lead to the activation of coagulation pathways. SARS-CoV-2 entry via ACE-2 receptors on endothelial cells is likely associated with endothelial dysfunction. This endotheliopathy plays a significant role in COVID-19 related microcirculatory changes [7]. Severe COVID-19, a hyperinflammatory state, is marked by elevated inflammatory markers including D-dimer, ferritin, IL-6, LDH, and CRP levels. Elevated D-dimer levels have been correlated with disease severity and poor outcomes in hospitalized patients with COVID-19 [8]. The incidence of VTE and pulmonary embolism among COVID-19 ICU patients was higher in a study from France [9]. The patient population who received the escalated dose of LMWH in our study either had SIC score ≥ 4 or D-dimer ≥ 2.2 (FEU). This data indicated that the median value of peak inflammatory markers in cohort 1 was lower (p<0.05) when compared to cohort 2. Patients in cohort 2 were sicker than cohort 1, as evidenced by a statistically significant longer length of hospital stay and a higher rate of ICU admission. However, the potential dose-dependent anti-inflammatory effect of LMWH was not observed. Additional studies evaluating comorbidities and disease severity in both cohorts may yield different results.
Conclusion:Aside from the known anticoagulant benefit of LMWH, there was no additional anti-inflammatory role with higher doses (1mg/kg/subcutaneously every 12 hours) of LMWH.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.